Menopause and the utilization of menopause hormone therapy (MHT) in Brazil
►Conteúdo gerado por Humano (a) para Humanos (as)◄
Claudio Santiago Dias Jr
Doutor em Demografia
Departamento de Sociologia/UFMG
Currículo Lattes: http://lattes.cnpq.br/1639549869923899
Brazilian women’s menopausal experiences
Women in menopause in Brazil have a diverse range of experiences and traits, as evidenced by several studies. Climactic symptoms are common, with 87.9% of women reporting symptoms including heat waves, which often appear around the age of 47 (Pompei et al, 2022). The prevalence of headaches, particularly migraines, is remarkable in postmenopausal women, with 14.7% suffering from migraines and 86.2% reporting some sort of past headache, many of which linger after menopause (Carturan et al, 2016). Interestingly, despite the high incidence of climatic symptoms, only a small fraction of Brazilian women begins hormone replacement therapy (HRT), and the average treatment duration is less than a year, with differences depending on socioeconomic level (Pompei et al, 2022).
Dimension of menopause and hormone use in Brazil
The Figure 1 displays the distribution of menopausal women aged 50 and up in Brazil. According to the data, 94.6% of women in this age group have had menopause, while 5.4% have not. This implies that menopause affects almost all Brazilian women over the age of 50.
Figure 1 – Distribution of women aged 50 and over, according to menopause, Brazil (2019-2021)
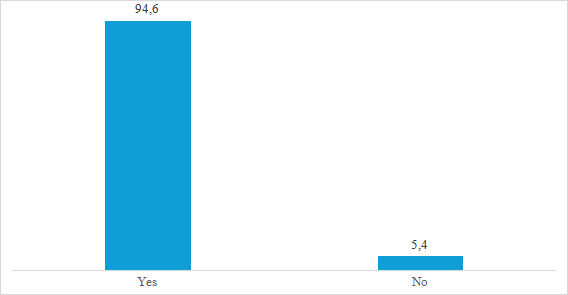
Source: Elsi-Brazil (2019-2021)
The cohort analysis categorizes women into four groups based on their current age: 50-59, 60-69, 70-79, and 80+. Within these cohorts, menopause initiation is compared across four initiation ages: before 45 years, between 45 and 49 years, between 50 and 54 years, and 55 years or more. In Cohort 1 (50-59), most women (94.31%) experienced menopause at 55 years or more, with the remaining percentages spread across earlier initiation ages. Cohort 2 (60-69) shows a diminishing later-onset category (93.19%), with the remaining cohorts seeing an increase in prevalence, particularly for menopause between 45 and 54 years. Cohort 3 (70-79) continues this trend, with the prevalence of later-onset menopause declining to 89.85% and earlier cohorts gaining representation. Finally, Cohort 4 (80+) sees a continuation of this shift, with later-onset menopause accounting for 83.86% and earlier cohorts further increasing. This data reveals a changing composition across current age groups, with earlier menopause instances becoming more noticeable over time, while later-onset menopause remains substantial, indicating its commonality.
Figure 2 – Menopause initiation prevalence by cohorts across current age groups
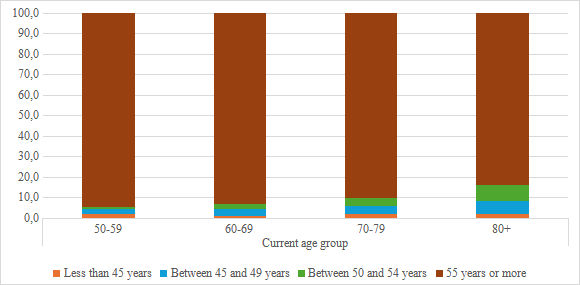
Source: Elsi-Brazil (2019-2021)
The data of Figure 3 provides insights into the distribution of menopausal women across different age groups and their engagement in hormonal treatment. It shows that most women across all age groups have not undergone hormonal treatment, with percentages ranging from 81.3% to 86.8%. The prevalence of women currently undergoing treatment diminishes with age, starting at 4.1% in the 50-59 age group and dropping to 0% in the 80+ group, reflecting a downward trend. Meanwhile, the proportion of women who have undergone treatment but no longer do increases initially, peaking at 16.8% in the 70-79 group, before declining to 13.2% in the 80+ group. This indicates a shift from current treatment to past treatment as women age, while the majority remain without hormonal intervention, highlighting a changing pattern of treatment engagement over time.
Figure 3 – Distribution of Hormonal Treatment Status Among Menopausal Women by Age Group
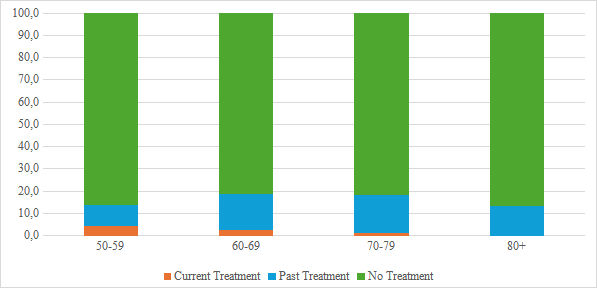
Source: Elsi-Brazil (2019-2021)
These findings highlight a changing pattern of treatment engagement over time and underscore the importance of considering age-related factors when discussing hormonal treatment for menopausal women. Future research should explore the reasons behind these trends, including changing attitudes toward hormonal therapy, healthcare accessibility, and medical guidance, to develop a more comprehensive understanding of the evolving dynamics of menopausal treatment engagement.
References
Carturan, P., Scorcine, C., & Fragoso, Y. D. (2016). Migraine in the post-menopausal period is associated with higher levels of mood disorders, disability, and more menopausal symptoms. Arquivos de Neuro-Psiquiatria, 74(12), 999–1002. https://doi.org/10.1590/0004-282×20160153
Pompei, L. M., Bonassi-Machado, R., Steiner, M. L., Pompei, I. M., De Melo, N. R., Nappi, R. E., & Fernandes, C. E. (2022). Profile of Brazilian climacteric women: Results from the Brazilian Menopause Study. Climacteric, 25(5), 523–529. https://doi.org/10.1080/13697137.2022.2088276
[ Se você gostou desse artigo, deixe um comentário. Além disso, compartilhe esse post em suas redes sociais, assim você ajuda a socializar a informação socioambiental ]
A manutenção da revista eletrônica EcoDebate é possível graças ao apoio técnico e hospedagem da Porto Fácil.
[CC BY-NC-SA 3.0][ O conteúdo da EcoDebate pode ser copiado, reproduzido e/ou distribuído, desde que seja dado crédito ao autor, à EcoDebate com link e, se for o caso, à fonte primária da informação ]